Information about a Colonoscopy
What is a colonoscopy?
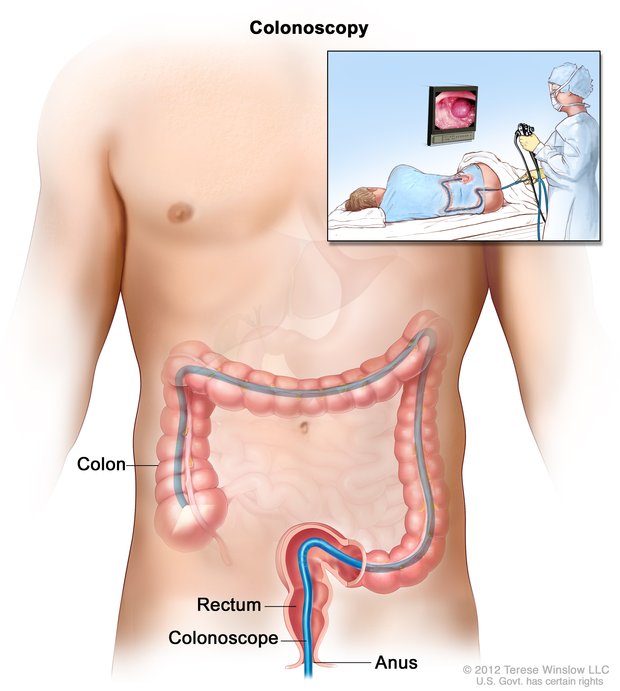
A colonoscopy is a test which will enable us to visualize your large bowel with a thin flexible tube which contains a video camera for optimal assessment. This will require that your bowel has been adequately cleansed. During the procedure biopsies may be performed for further analysis and polyps may be removed.
A colonoscopy is currently the most accurate technique for detecting lesions in the colon. Other modalities however have been utilized as alternatives. These include a virtual colonoscopy, an x-ray technique which still involves the same bowel preparation as that which is necessary for a normal colonoscopy. In addition no samples can be taken with this technique. Hence a full colonoscopy may be necessary if a lesion is found. In addition a virtual colonoscopy misses approximately 10-30% of significant polyps and a significant amount of air is instilled in the bowel during the procedure which may be associated with significant discomfort. Testing for blood in the faeces may have been performed prior to your colonoscopy, but this is a screening test only.
A colonoscopy is an accurate test for detecting diseases of the colon and in particular bowel cancer, it will detect between 97 and 99% of bowel cancers according to the studies that have been performed, hence there is a small chance of missing a bowel cancer and thus it is very important that this risk is diminished by you adequately cleansing the bowel as instructed and we will endeavour to minimize the risk by performing complete examination of the bowel and utilizing techniques to assist us in visualizing the bowel mucosa.
The Risks of Colonoscopy
There are three broad categories of risks associated with having a colonoscopy. The first is those that are associated with the preparation. The second, those that are associated with the anaesthetic, and the third those that are associated with the colonoscopy itself. Each will be covered in a point-like format to assist with your understanding of these risks.
A. Colonic Preparation.
The preparation is generally well tolerated. However crampy pain, nausea and vomiting may occur. Uncommonly more significant problems such as dizziness and fainting may result from the preparation. If you have had problems with previous preparations for colonoscopy assessments, please feel free to discuss these issues with us prior to the procedure, and we may alter your preparation accordingly. Importantly the presence of another responsible adult in your home whilst you are being prepared is very important and if such cannot be arranged, again please discuss this with us prior to your colonoscopy.
B. Anaesthetic Risks
There are a number of anaesthetic risks associated with the procedure which include bruising or infection at the cannula site, allergic reactions, aspiration of vomit, heart attacks or strokes. Extremely rarely death can result from the anaesthetic. If you have any questions with regards to the above anaesthetic risks, please feel free to discuss these with the anaesthetist prior to the procedure. Clearly however in general terms the anaesthetic is safe and well tolerated.
C. Colonoscopy Risks
A colonoscopy in general is a very safe procedure. However there are some risks that you should be aware of prior to having this procedure. The first is that of bleeding which is very rare following a normal colonoscopy without removal of a polyp. However if a polyp is removed the risk increases to approximately 1 in every 1,000 cases, and if it is a large polyp this increases to between 1 and 3 in every 100 cases. This risk is significantly increased in patients who are on blood thinning medications, and hence you may be required to cease these prior to the procedure. If these are continued large polyps may not be able to be removed at the time of your colonoscopy. If bleeding was to occur, a hospital admission may be required and during this admission you may require a blood transfusion, a further colonoscopic assessment to try and arrest the bleeding, and rarely an operation may be required to control the bleeding.
Perforation is also infrequent following a standard colonoscopy. However the data has demonstrated that this occurs in approximately 1 in every 3,000 procedures. This may be detected at the time of your colonoscopy and subsequently may be treated during the colonoscopy with clips, or it may be undetected until following the colonoscopy at which point you may have severe pain in the abdomen. In either case a hospital admission would be required and an operation is often necessary. Finally, rarely other complications may occur such as damage to other organs in the abdomen which again may require hospital admission and need surgical intervention.
What to do before your Colonoscopy
There are a number of variables which may alter the way your procedure is performed. Hence it is important that we obtain accurate information from you prior to the colonoscopic assessment and its associated preparation so that we can optimally treat you. One of the most important areas that we may need to discuss with you is what medications you are on. You should continue with all your usual medications, except those that are specified below.
Diabetic MedicationsIf you are on diabetic medications you will need to discuss this with us. A protocol may be established for you by your General Practitioner, Endocrinologist or Dr Lynch prior to your procedure.
Warfarin TherapyThe indications for the use of warfarin vary from patient to patient, and hence this issue needs to be discussed with your Medical Practitioner (and this may include your Cardiologist) prior to the procedure. If the warfarin is to be ceased, this should be done at least 3 days prior to the procedure and you should have a blood test (INR) prior to the procedure which you should discuss with us. A colonoscopy can still be performed whilst on warfarin therapy, assuming that the warfarin cannot be ceased, however the removal of a large polyp under such circumstances would not be possible, and this problem may need to be addressed at a later date following discussion with Dr Lynch.
Other blood thinning agents, may need to be ceased prior to the procedure. These medications however may be very important for other conditions that you are suffering from (in particular cardiac stents) and the cessation of these should only be performed after discussion with your Medical Practitioners, which may include your Cardiologist. In addition, Dr. Lynch is more than happy to discuss these issues with you prior to your procedure. Again if these medications cannot be ceased, a large polyp cannot subsequently be removed and further management of this situation will need to be discussed with you. It is important to note that Aspirin can be continued up until the time of your colonoscopy.
Miscellaneous MedicationsIron tablets because of their blackening effect should be stopped at least 7 days before the procedure. If you are taking any herbal medications this should be discussed with us prior to the procedure. Fish oil should be ceased 7 days before the procedure because of its blood thinning properties.
Heart ProblemsYou may require antibiotics with your procedure, in particular if you have cardiac valve disorders or a history of infection of the heart valves or following certain types of surgery on your vascular system. Please inform us of any of the above. Also if you have a pacemaker or an implanted defibrillator please inform us of these prior to your procedure.
Kidney DiseaseIf you have a history of kidney disease this may alter the preparation that you will require for your procedure, and hence we will need to know this before the colonoscopic assessment.
What can I expect after the Colonoscopy?
Following the colonoscopy you will go to the recovery area where initially you will be placed on a bed, and this will be followed by being seated. You will gradually recover during this period of time and will subsequently be discharged when the nursing staff feel that your recovery is adequate. You will need to have an adult accompanying you home and stay with you for the next 12hrs. Following discharge you will be able to eat normally and take your regular medications unless otherwise specified. As a result of the anaesthetic agents that you have had, for 12hrs following the procedure you must not drive a vehicle, operate heavy machinery or sign legal documents or place yourself in any hazardous situation. Basically plan to take it easy and relax for the rest of the day.
Following the procedure you may suffer from bloating and cramping discomfort in the abdomen which will normally settle over a few hours. Occasionally you can have diarrhoea for a 24hr period following the colonoscopy. Uncommonly it can last longer than this. Also occasionally constipation may occur for a few days following the procedure. Haemorrhoids may be flared by the procedure with subsequent bleeding and topical agents can be utilized for haemorrhoids. If following the procedure you have severe abdominal pain, bleeding from the back passage (greater than a few tablespoons) black bowel motions, high fever or other concerning symptoms you are to contact your local doctor, Dr Lynch or the Accident & Emergency Department of your local hospital.
You may be asked to see Dr Lynch again in consultation, and this will generally be arranged prior to your discharge. Other investigations may also be ordered. Your referring doctor will receive a letter of correspondence relating to the colonoscopy, and you should make an appointment to see your referring doctor within a week of the procedure unless otherwise specified.
How to Prepare for your Colonoscopy
For patients using Picoprep only* please choose the day of your procedure below:
Information for patients with a colonoscopy on Wednesday using Picoprep only.
- Brown bread
- High fibre
- Vegetables
- Fruit
- Any food containing seeds or nuts, yellow cheese.
Please choose what you like from the following menu:
Breakfast:- Fruit juice (apple or pear)
- Corn flakes or rice bubbles with milk
- Eggs (boiled, scrambled or omelette)
- White bread or toast with margarine or butter, honey or vegemite.
- Clear fruit juice (apple or pear)
- Clear chicken soup
- White bread sandwich with any of these fillings - chicken, beef, fish, egg.
- Stewed or tinned fruit without skin
- Tea and coffee with milk and sugar Dinner:
- Steamed or grilled lean meat - chicken or fish
- Lean beef or lamb
- Mashed or boiled peeled potato, peeled pumpkin or choko.
- White rice or plain noodles or white pasta
- Stewed or tinned fruit (without skins) with ice cream
- Clear fruit juice (apple or pear), ginger ale, tea or coffee Mid Meals:
- Tea, coffee, apple or pear juice, lemonade
- Plain biscuit (eg Jatz, Sao, Morning Coffee, Milk Arrowroot) plain sponge cake, crumpet, yoghurt, custards or plain jelly.
Low fibre Breakfast Before 8am. After 8am approved fluids only.
Approved fluids:- Water
- Apple or pear juice
- Plain jelly
- Black tea or coffee
- Bonox
- Lucozade
- Gatorade
- Staminade
- Carbonated drinks
- Barley sugar drink
- Clear broth
- Lime or lemon cordial
- Dairy Products (milk, plain ice cream & plain yoghurt)
Drink at least 3 litres of approved clear fluids plus the preparation liquids.
2pm FIRST DOSE OF PREPARATIONAdd the contents of one sachet of Picoprep to one glass (250ml) of warm water and stir until dissolved. Chill for 30 minutes before drinking if you prefer. This should be followed by a drink from any of the approved clear fluids (see above).
6pm SECOND DOSE OF PREPARATIONAdd the contents of one sachet of Picoprep to one glass (250ml) of warm water and stir until dissolved. Chill for 30 minutes before drinking if you prefer. This should be followed by a drink from any of the approved clear fluids (see above).
After a short time the preparations will cause multiple bowel movements, resulting in diarrhoea and watery stools. DO NOT LIE DOWN for at least 2 hours after drinking the mixture; you may sit down but ensure your torso is upright for maximum effect. Walking around will increase itʼs effectiveness in clearing the large intestine.
From the time you start your first preparation do not leave the house and stay close to the bathroom.
Add the contents of one sachet of Picoprep to one glass (250ml) of warm water and stir until dissolved. Chill for 30 minutes before drinking if you prefer. This should be followed by a drink from any of the approved clear fluids (see above).
CAN CONTINUE TO DRINK CLEAR FLUIDS ( FROM APPROVED LIST) UNITL 3 HOURS PRIOR TO YOUR APPOINTMENT TIME - THEN NIL BY MOUTH FROM THEN ON - NOTHING TO EAT OR DRINK.Information for patients with a colonoscopy on Wednesday using Picoprep only.
- Brown bread
- High fibre
- Vegetables
- Fruit
- Any food containing seeds or nuts, yellow cheese.
Please choose what you like from the following menu:
Breakfast:- Fruit juice (apple or pear)
- Corn flakes or rice bubbles with milk
- Eggs (boiled, scrambled or omelette)
- White bread or toast with margarine or butter, honey or vegemite.
- Clear fruit juice (apple or pear)
- Clear chicken soup
- White bread sandwich with any of these fillings - chicken, beef, fish, egg.
- Stewed or tinned fruit without skin
- Tea and coffee with milk and sugar Dinner:
- Steamed or grilled lean meat - chicken or fish
- Lean beef or lamb
- Mashed or boiled peeled potato, peeled pumpkin or choko.
- White rice or plain noodles or white pasta
- Stewed or tinned fruit (without skins) with ice cream
- Clear fruit juice (apple or pear), ginger ale, tea or coffee Mid Meals:
- Tea, coffee, apple or pear juice, lemonade
- Plain biscuit (eg Jatz, Sao, Morning Coffee, Milk Arrowroot) plain sponge cake, crumpet, yoghurt, custards or plain jelly.
Low fibre Breakfast Before 8am. After 8am approved fluids only.
Approved fluids:- Water
- Apple or pear juice
- Plain jelly
- Black tea or coffee
- Bonox
- Lucozade
- Gatorade
- Staminade
- Carbonated drinks
- Barley sugar drink
- Clear broth
- Lime or lemon cordial
- Dairy Products (milk, plain ice cream & plain yoghurt)
Drink at least 3 litres of approved clear fluids plus the preparation liquids.
2pm FIRST DOSE OF PREPARATIONAdd the contents of one sachet of Picoprep to one glass (250ml) of warm water and stir until dissolved. Chill for 30 minutes before drinking if you prefer. This should be followed by a drink from any of the approved clear fluids (see above).
6pm SECOND DOSE OF PREPARATIONAdd the contents of one sachet of Picoprep to one glass (250ml) of warm water and stir until dissolved. Chill for 30 minutes before drinking if you prefer. This should be followed by a drink from any of the approved clear fluids (see above).
After a short time the preparations will cause multiple bowel movements, resulting in diarrhoea and watery stools. DO NOT LIE DOWN for at least 2 hours after drinking the mixture; you may sit down but ensure your torso is upright for maximum effect. Walking around will increase itʼs effectiveness in clearing the large intestine.
From the time you start your first preparation do not leave the house and stay close to the bathroom.
Add the contents of one sachet of Picoprep to one glass (250ml) of warm water and stir until dissolved. Chill for 30 minutes before drinking if you prefer. This should be followed by a drink from any of the approved clear fluids (see above).
CAN CONTINUE TO DRINK CLEAR FLUIDS ( FROM APPROVED LIST) UNITL 3 HOURS PRIOR TO YOUR APPOINTMENT TIME - THEN NIL BY MOUTH FROM THEN ON - NOTHING TO EAT OR DRINK.Information for patients with a colonoscopy on Friday using Picoprep only.
- Brown bread
- High fibre
- Vegetables
- Fruit
- Any food containing seeds or nuts, yellow cheese.
Please choose what you like from the following menu:
Breakfast:- Fruit juice (apple or pear)
- Corn flakes or rice bubbles with milk
- Eggs (boiled, scrambled or omelette)
- White bread or toast with margarine or butter, honey or vegemite.
- Clear fruit juice (apple or pear)
- Clear chicken soup
- White bread sandwich with any of these fillings - chicken, beef, fish, egg.
- Stewed or tinned fruit without skin
- Tea and coffee with milk and sugar Dinner:
- Steamed or grilled lean meat - chicken or fish
- Lean beef or lamb
- Mashed or boiled peeled potato, peeled pumpkin or choko.
- White rice or plain noodles or white pasta
- Stewed or tinned fruit (without skins) with ice cream
- Clear fruit juice (apple or pear), ginger ale, tea or coffee Mid Meals:
- Tea, coffee, apple or pear juice, lemonade
- Plain biscuit (eg Jatz, Sao, Morning Coffee, Milk Arrowroot) plain sponge cake, crumpet, yoghurt, custards or plain jelly.
Low fibre Breakfast Before 8am. After 8am approved fluids only.
Approved fluids:- Water
- Apple or pear juice
- Plain jelly
- Black tea or coffee
- Bonox
- Lucozade
- Gatorade
- Staminade
- Carbonated drinks
- Barley sugar drink
- Clear broth
- Lime or lemon cordial
- Dairy Products (milk, plain ice cream & plain yoghurt)
Drink at least 3 litres of approved clear fluids plus the preparation liquids.
2pm FIRST DOSE OF PREPARATIONAdd the contents of one sachet of Picoprep to one glass (250ml) of warm water and stir until dissolved. Chill for 30 minutes before drinking if you prefer. This should be followed by a drink from any of the approved clear fluids (see above).
6pm SECOND DOSE OF PREPARATIONAdd the contents of one sachet of Picoprep to one glass (250ml) of warm water and stir until dissolved. Chill for 30 minutes before drinking if you prefer. This should be followed by a drink from any of the approved clear fluids (see above).
After a short time the preparations will cause multiple bowel movements, resulting in diarrhoea and watery stools. DO NOT LIE DOWN for at least 2 hours after drinking the mixture; you may sit down but ensure your torso is upright for maximum effect. Walking around will increase itʼs effectiveness in clearing the large intestine.
From the time you start your first preparation do not leave the house and stay close to the bathroom.
Add the contents of one sachet of Picoprep to one glass (250ml) of warm water and stir until dissolved. Chill for 30 minutes before drinking if you prefer. This should be followed by a drink from any of the approved clear fluids (see above).
CAN CONTINUE TO DRINK CLEAR FLUIDS ( FROM APPROVED LIST) UNITL 3 HOURS PRIOR TO YOUR APPOINTMENT TIME - THEN NIL BY MOUTH FROM THEN ON - NOTHING TO EAT OR DRINK.*If you were advised (by Coast Endoscopy) to use an alternate preparation (not picoprep), please contact us for preparation information
Information for Diabetic patients
As a diabetic patient it is important that your procedure is coordinated carefully and hence you are required to discuss the timing of your medication and the timing of your procedure with the Coast Endoscopy staff.
If you are on oral hypoglycaemics:- No tablets taken evening before colonoscopy. No tablets on day of procedure.
- Take morning tablets as per usual on the day before procedure
- 1/2 dosage on the night before colonoscopy. No insulin on day of procedure.
- Take normal morning dose on the day before the procedure
- Low fibre breakfast on day before procedure.
- Bring insulin on day of colonoscopy so it can be administered after procedure.
Requirements
Approximately 1 week before your Procedure:
- Medicare Card, Health Fund, DVA & Pension Details
- Referral from your GP (fax 07 5599 2293 or email to admin@coastendoscopy.com.au)
- Tweed Day Surgery paperwork (click here to complete online)
- Call us on 07 5599 2295 to determine which preparation to use
- Purchase preparation from us or buy from your pharmacy
- View and follow your diet and preparation information (see preparation tab above)
- Ensure you have a driver. The patient must not drive on the day of their procedure.
- Payment (eg. Credit Card) for Tweed Day Surgery